Research
History of Development
Children’s heart disease—congenital heart disease
One in 100 children are born with a congenital heart disease, a congenital abnormality of the heart structure.
That means, 8,000 babies are born with congenital heart disease every year across Japan.
Including both children and adults, there are over 600,000 patients with congenital heart disease in Japan.
Treatment for congenital heart disease is characterized by the fact that the heart to be treated is very tiny compared with adults’ because the patients are newborns or infants, there are many types of diseases, and the three-dimensional structure of the heart is complex and varies depending on the patient or disease type.
Therefore, cardiac surgery, which is the major treatment approach, requires extremely difficult techniques.
Conventionally, a pediatrician diagnoses a patient based on echocardiography, cardiac catheterization study, and cardiac CT and MRI studies and reports the diagnosis to a cardiac surgeon.
Most of these imaging studies provide two-dimensional images. Therefore, information given to surgeons is not sufficient to accurately understand the abnormalities of the hearts of patients with congenital heart disease, which is characterized by a complex three-dimensional structure.
Although multi-slice CT and cardiac MRI studies have recently made it possible to create 3D-like images of the heart structure, they are still 2D images to which shades are added to show them as if they are 3D images. Therefore, it is difficult to understand the complex structure of patient’s heart based on these images displayed on a screen.
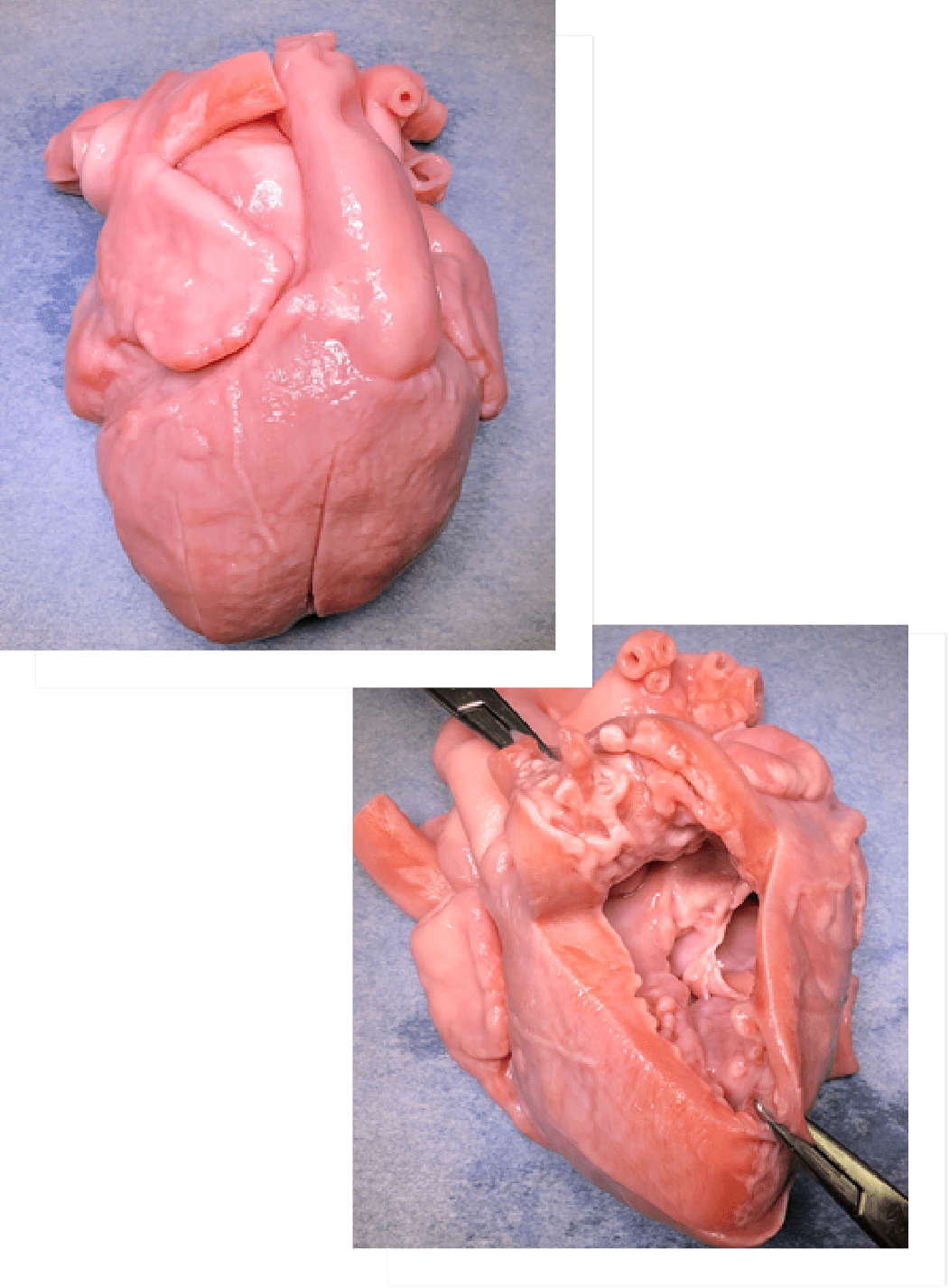
We believe that it is necessary to create heart replicas of the same size, shape and texture as actual patients’ hearts in order to provide information that will allow surgeons to quickly and accurately understand complex heart structures.
Movie: Surgery simulation using a heart replica
Development of Heart Replica
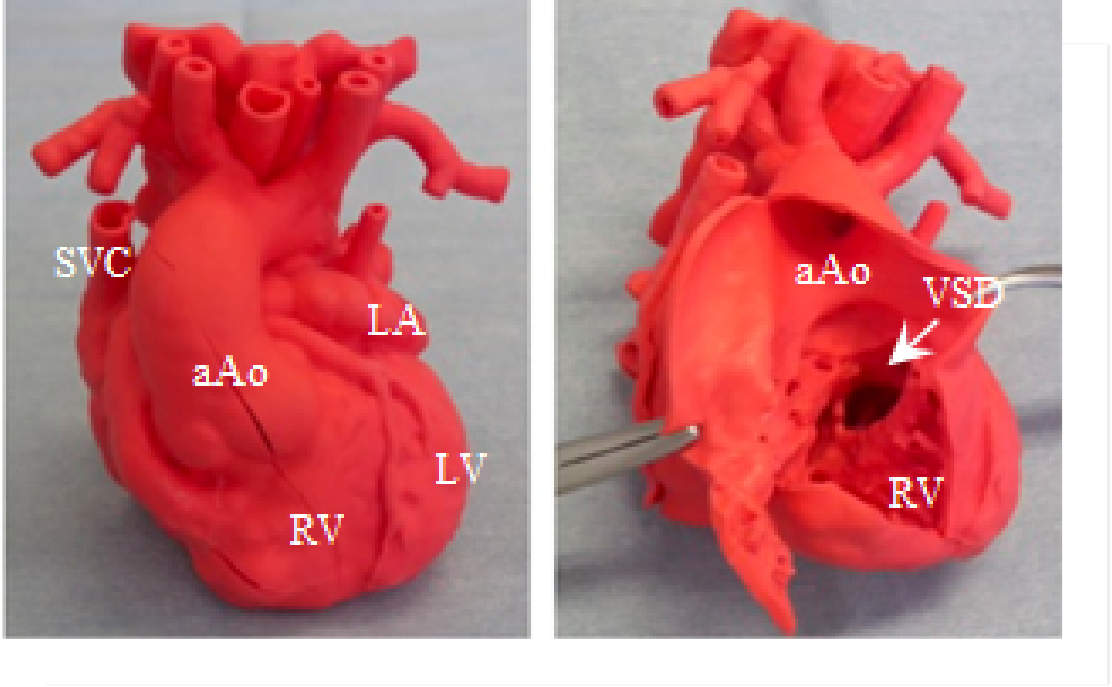
About 20 years ago, we started to explore a way to apply 3D printing technology, which was starting to become common in industry at that time, to creating heart replicas. Initially, we created a rigid plastic heart replica using a 3D printer and reported its usefulness. However, it could not be used for surgery simulation (surgery rehearsal) because it could not be cut or sutured due to its stiffness. We then looked for a company with the technology required for creating soft heart replicas that can be cut and sutured and accurately reproduce actual patients’ hearts.
We started a joint research and development project with CrossMedical, Inc. in 2010. In the course of that project, we successfully developed a full-scale, flexible, super-soft and finely-detailed polyurethane heart replica that can be cut and sutured. The replicas are based on 3D image data of a patient’s heart by combining stereolithography, a precise 3D printing technology, with the vacuum injection method, a special casting technology. In 2020, the pre-market application for this replica was accepted and the replica became available in clinical practice across Japan. A physician-initiated clinical trial was completed in 2021. At present, we are preparing to apply for insurance coverage for this heart replica.
We have also jointly developed a novel ultraviolet-curable inkjet 3D printer with SCREEN Holdings and Kyoeisha Chemical, aiming at shortening the time and reducing costs for creating heart replicas. This replica is called a wet-type heart replica because it is kept wet during storage. It can reproduce very fine structures inside and outside the heart because it is created without using a mold.
Development of ped UT-Heart
The complexity of congenital heart disease arises not only from the heart structure but also the blood flow. Abnormalities of the heart structure including large holes in the heart or differences in the diameters of the great vessels can cause abnormal blood flow such as regurgitation.
To achieve more successful treatment for congenital heart disease, it is necessary to give accurate and detailed information on complex blood flows associated with abnormal heart structures in addition to developing a simulator that accurately reproduces complex heart structures. Further support for difficult surgeries for patients with congenital heart disease will be possible if the cardiac blood flows of these patients can be reproduced in detail, and post-operative blood flows can be predicted by making maximum use of image processing and computing technologies.
The University of Tokyo and UT-Heart Inc. has jointly developed a multi-scale/multi-physics heart simulator UT-Heart (for adults) that accurately reproduces the cardiac motion of individual patients on a computer. Heart models reproduced on a computer allow surgeons to try several treatment options on a computer and to offer their patients the best option as well as help them understand disease of their patients. Application of this system to pediatric patients with congenital heart disease may allow surgeons to offer the best treatment option for individuals by virtually performing various types of surgeries on a computer before actual surgery.
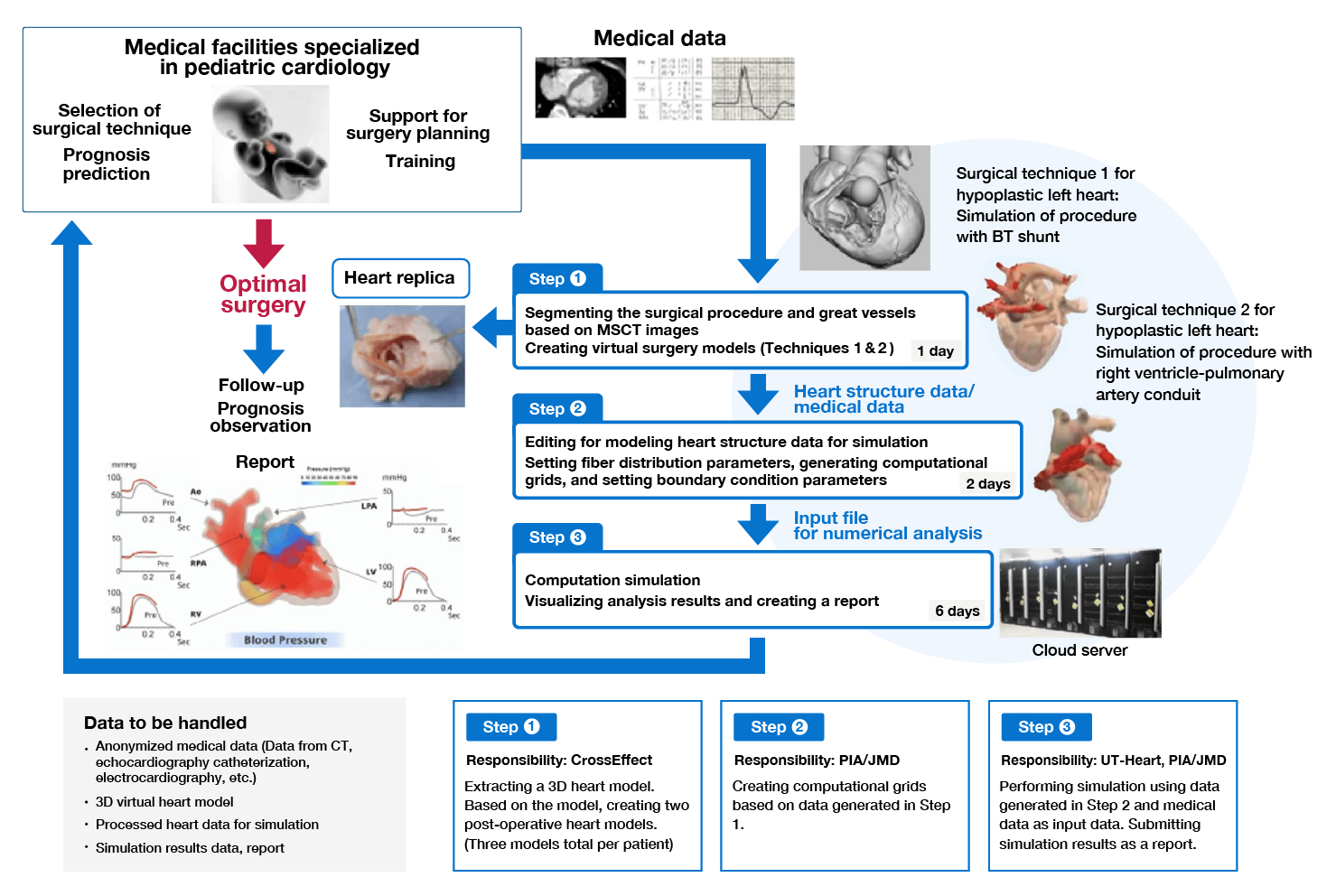
To apply the UT-Heart developed for adult patients to supporting treatment for pediatric patients with congenital heart disease which is characterized by small and complex 3D heart structure, we have developed a new simulator, ped UT-Heart, in cooperation with Japan Medical Device Corporation and PIA Corporation Inc. A clinical study of this newly-developed ped UT-Heart is now being conducted to examine whether can help lead to the selection of optimal surgical techniques and treatment strategies in pediatric patients with congenital heart disease.
Simulation process with ped UT-Heart
The heart simulator UT-Heart is modified to develop ped UT-Heart, which is intended to be used in combination with a 3D realistic heart replica for the treatment of pediatric patients with congenital heart disease.
By performing virtual surgeries on a computer and predicting post-operative hemodynamics with ped-UT Heart, surgeons will be able to offer surgical techniques that are optimal for ensuring the QoL of each patient. Conventionally, surgeons had no choice but to select a surgical technique based on intuition. Through the development of ped-UT Heart, we will help surgeons select the best surgical technique on a reasonable basis to maintain good QoL of pediatric patients throughout their lives.